Lumbar Degenerative Disc Disease
What is lumbar degenerative disc disease (discogenic pain)?
Lumbar intervertebral discs are a common cause of chronic low back pain. A fissure (tear) in the outer fibrous portion of the disc, the annulus fibrosus, can allow some of the inner “jelly-like” portion, the nucleus pulposus, to leak out. This can lead to chronic inflammation, ingrowth of nerves into the disc, and increased sensitization and subsequent pain emanating from the disc. The gold standard method for diagnosis of painful lumbar degenerative disc disease (lumbar discogenic pain) is provocative lumbar discography.
What are common features of lumbar degenerative disc disease (discogenic pain)?
Patients with painful lumbar degenerative disc disease (lumbar discogenic pain) typically complain of deep and aching low back pain that can become sharp with movement, an inability to sit for prolonged periods of time, temporary relief with change of position, and low back more than leg pain. This type of low back pain commonly begins with a lifting and/or twisting injury.
How is lumbar degenerative disc disease (discogenic pain) diagnosed?
Painful lumbar degenerative disc disease (lumbar discogenic pain) is typically diagnosed via a combination of findings from the history, physical examination, and advanced imaging (MRI, CT). However, we must also be mindful that >60% of people without any low back pain whatsoever will have disc changes on advanced imaging and, as such, we cannot rely too heavily on imaging findings alone to formulate a diagnosis. MRI findings such as a high intensity zone or Modic changes have a high specificity (87% and 70%, respectively) for painful lumbar degenerative disc disease (lumbar discogenic pain). In the end, though, the gold standard for diagnosis of painful lumbar degenerative disc disease (lumbar discogenic pain) remains provocative lumbar discography.

How is lumbar degenerative disc disease (lumbar discogenic pain) treated?
Initial treatment options for management of painful lumbar degenerative disc disease (lumbar discogenic pain) may include medications, physical therapy, and/or chiropractic. In many cases, these conservative measures will allow for excellent recovery. If a patient is still experiencing significant pain despite the aforementioned treatment options, epidural steroid injections may be considered to decrease the inflammatory component of the pain. Alternative interventional options may include intradiscal platelet-rich plasma (PRP) injections. If all conservative measures have been exhausted, referral to spine surgery for consideration of fusion surgery may then be considered.
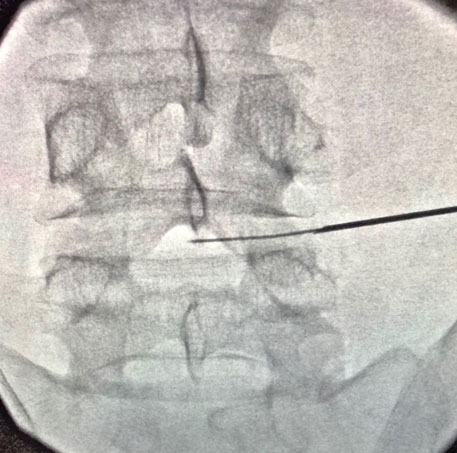
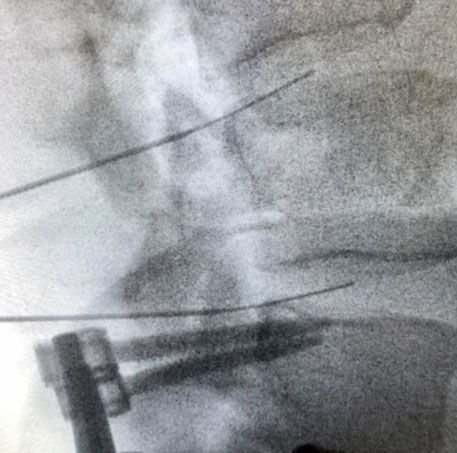
Provocative Lumbar Discography
Provocative lumbar discography is the gold standard diagnostic test to precisely confirm or exclude the intervertebral disc as a source of chronic low back pain. Using fluoroscopic (x-ray) guidance, needles are placed within two or more discs and pressurized using contrast dye. Based on patient response (i.e. whether the patient’s typical low back pain is reproduced or not) and imaging findings such as fissures (tears) within the disc(s), a diagnosis of painful lumbar degenerative disc disease (lumbar discogenic pain) can be confirmed or ruled out as a source of chronic low back pain.
Patients who have been experiencing low back pain for greater than 3 months, have tried and failed conservative management (medications, physical therapy, chiropractic), and for whom non-invasive diagnostic tests (x-ray, MRI) have failed to precisely diagnose the source of low back pain.
Low back pain is a very common cause of musculoskeletal disability, but “low back pain” is not a diagnosis. There are distinct anatomic spinal structures that can potentially generate pain. Studies have shown that the intervertebral discs are the main pain generating structure in 40-70% of cases of axial (non-radiating) low back pain. In patients younger than 60 years of age, the disc is the most common cause of low back pain, followed by the sacroiliac joint then the facet joint. In patients older than 60 years of age, the facet joint is the most cause of low back pain, followed by the disc then the sacroiliac joint. As such, provocative lumbar discography is an important tool to precisely diagnose pain emanating from the lumbar intervertebral discs.
Despite concerns raised by some physicians that lumbar discography contributes to higher rates of disc degeneration, a recent review of the safety and overall diagnostic value of provocative lumbar discography concluded that it is a safe and helpful diagnostic test when performed by properly trained physicians using strict procedural guidelines as outlined by the Spine Intervention Society.
First, in patients who eventually go on to have lumbar fusion surgery for management of their painful lumbar degenerative disc disease (lumbar discogenic pain), there is an 88% chance of success with a positive discogram compared to just a 50% chance of success with a negative discogram. Second, when lumbar discography identifies the source of a patient’s low back pain earlier in their clinical course, it can save the patient from potentially excessive and unnecessary testing and treatment. Lastly, it can potentially provide peace of mind by having a precise diagnosis of one’s low back pain.
Intradiscal Platelet Rich Plasma (PRP)
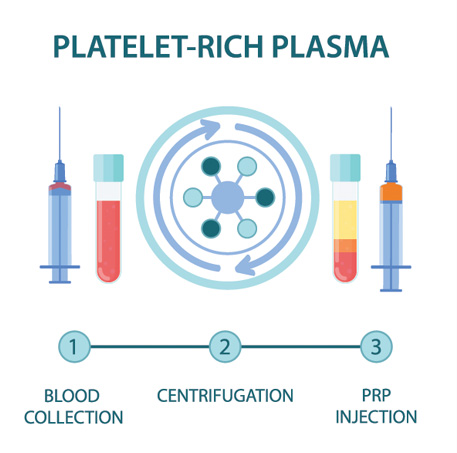
PRP is component of the patient’s own blood. It is rich in growth factors and other cells that signal an increased healing response to a damaged tissue. It is used to treat a variety of painful spine and musculoskeletal conditions.
Blood is drawn from a patient and then placed in a centrifuge for it to be “spun down.” This causes the different components of the blood to separate out in the vial. The PRP solution is then drawn up into a syringe and prepared to be injected at the site of the patient’s injury.
Discontinue use of all non-steroidal anti-inflammatory drugs (NSAIDs) at least 7 days prior to the procedure. These ay include ibuprofen (Advil, Motrin), naproxen (Aleve), meloxicam (Mobic), diclofenac (Voltaren), indomethacin (Indocin), and celecoxib (Celebrex). If you are taking oral corticosteroids such as prednisone or a Medrol Dosepak, please discuss this with Dr. Best prior to your procedure. In many cases, Dr. Best may request that the corticosteroid medication be discontinued in preparation for the PRP injection. Do NOT stop aspirin unless specifically instructed by Dr. Best. Depending which body part is injected, you may need a driver to and from your procedure. If you have any questions or concerns about whether to continue or discontinue any of your medications leading up to your PRP injection, please discuss these issues with Dr. Best and his team.
Once the PRP solution is created, the patient is positioned for the procedure. The skin is thoroughly cleaned and the target for the injection obtained with ultrasound or fluoroscopy (x-ray). Then, a numbing solution is injected at the skin and subcutaneous tissues for increased procedural comfort. Finally, under ultrasound or fluoroscopic (x-ray) guidance, the needle is guided to the injury site and the PRP solution is deposited.
It is common to experience mild to moderate pain or discomfort during the initial 0-3 days after the PRP procedure. Post-procedure pain can be easily managed with acetaminophen (Tylenol) or other non-NSAID pain medication. Try to avoid applying ice or heat to the injection site.
During the 3–14-day period after the PRP injection, you may gradually increase physical activity. Please continue to avoid use of NSAIDs; however, ice may be applied for short periods of time throughout the day to aid in management of post-procedure soreness/discomfort if present.
During the 2–4-week period after the PRP, Dr. Best may recommend initiation of a course of physical therapy to aid in recovery and optimization of healing. The patient may begin to note improvement in pain during this time period, though it often takes 1 month or more for the benefits of PRP to take hold.
At this time, PRP injections are not typically covered by any insurance companies. Pricing and payment options can be discussed with Dr. Best and his team prior to your procedure.
At a Glance
Dr. Craig Best
- Harvard Fellowship-Trained Interventional Spine & Sports Medicine Specialist
- Double Board-Certified in Physical Medicnie & Rehabilitation and Pain Medicine
- Assistant Professor of Physical Medicine & Rehabilitation and Orthopedic Surgery
- Learn more

