Femoroacetabular Impingement (FAI)
What is femoroacetabular impingement?
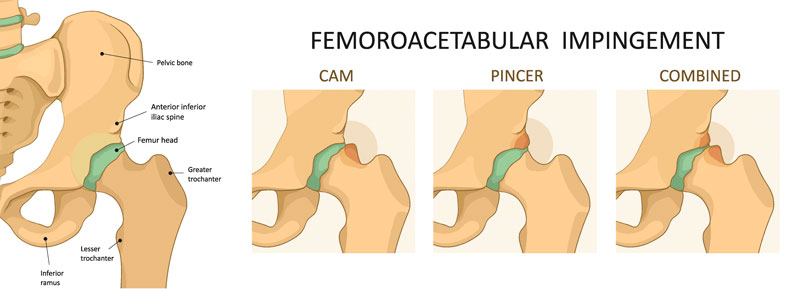
The hip joint is a “ball and socket” joint. The femoral head portion comprises the “ball” while the acetabulum comprises the “socket.” Femoroacetabular impingement (FAI) occurs when there is pathologic or abnormal contact of bony prominences of the hip joint during range of motion. This can be a major cause of early onset osteoarthritis, particularly in young athletic patients.
There are three types of FAI. Cam impingement occurs when there is excessive bony growth at the junction of the femoral head and neck (“ball” aspect of the ball and socket joint). Pincer impingement occurs when there is overgrowth of the acetabulum (“socket” aspect of the ball and socket joint). Mixed impingement is a combination of cam and pincer types. In all three scenarios, there is excessive and abnormal contact of bony prominences of the femoroacetabular joint which can lead to cartilage delamination and labral tears with subsequent increased risk of early onset arthritic changes.
What are the clinical features of femoroacetabular impingement?
Patients with FAI commonly present with anterior (front) hip and groin pain that is worsened with prolonged sitting, hip rotation, or sports/exercise activities. Physical examination may reveal limited and painful hip internal rotation and positive impingement testing.
How is femoroacetabular impingement diagnosed?
Diagnosis of FAI includes history and physical examination findings as noted above. Imaging with x-ray, CT, and/or MRI can help to evaluate for structural and morphologic findings to aid in the diagnosis of FAI and commonly associated findings such as labral tears. Diagnostic hip injections with local anesthetic may also play a role in more conclusively ruling in or ruling out the hip joint as a source of pain.
How is femoroacetabular impingement treated?
Initial treatment options for management of FAI may include medications and physical therapy. Physical therapy should primarily focus on multi-planar hip, gluteal, and core strength and stability. If a patient is still experiencing significant pain despite the aforementioned treatment options, interventional options may include corticosteroid or platelet rich plasma (PRP) injections. Finally, referral to orthopedic surgeon skilled in hip arthroscopy may be considered for further evaluation and consideration of surgical intervention.
Hip Joint Injection
Using x-ray (fluoroscopic) or ultrasound, a needle is carefully and precisely guided to the hip joint. Once the hip joint capsule has been accessed, a steroid solution is instilled through the needle and into the joint. This helps to decrease inflammation and, subsequently, decreases pain and improves function.
Platelet Rich Plasma (PRP)
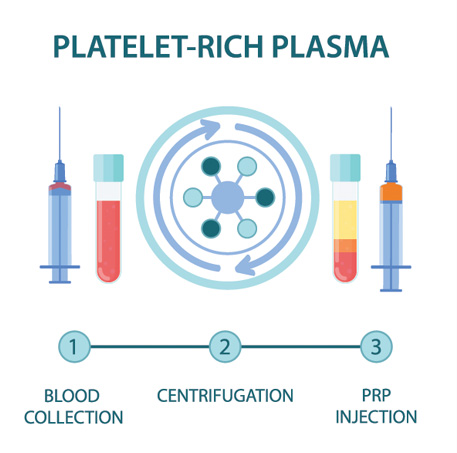
PRP is component of the patient’s own blood. It is rich in growth factors and other cells that signal an increased healing response to a damaged tissue. It is used to treat a variety of painful spine and musculoskeletal conditions.
Blood is drawn from a patient and then placed in a centrifuge for it to be “spun down.” This causes the different components of the blood to separate out in the vial. The PRP solution is then drawn up into a syringe and prepared to be injected at the site of the patient’s injury.
Discontinue use of all non-steroidal anti-inflammatory drugs (NSAIDs) at least 7 days prior to the procedure. These may include ibuprofen (Advil, Motrin), naproxen (Aleve), meloxicam (Mobic), diclofenac (Voltaren), indomethacin (Indocin), and celecoxib (Celebrex). If you are taking oral corticosteroids such as prednisone or a Medrol Dosepak, please discuss this with Dr. Best prior to your procedure. In some cases, Dr. Best may request that the corticosteroid medication be discontinued in preparation for the PRP injection. Do NOT stop aspirin unless specifically instructed by Dr. Best. Depending which body part is injected, you may need a driver to and from your procedure. If you have any questions or concerns about whether to continue or discontinue any of your medications leading up to your PRP injection, please discuss these issues with Dr. Best and his team.
Once the PRP solution is created, the patient is positioned for the procedure. The skin is thoroughly cleaned and the target for the injection obtained with ultrasound or fluoroscopy (x-ray). Then, a numbing solution is injected at the skin and subcutaneous tissues for increased procedural comfort. Finally, under ultrasound or fluoroscopic (x-ray) guidance, the needle is guided to the injury site and the PRP solution is deposited.
It is common to experience mild to moderate pain or discomfort during the initial 0-3 days after the PRP procedure. Post-procedure pain can be easily managed with acetaminophen (Tylenol) or other non-NSAID pain medication. Try to avoid applying ice or heat to the injection site.
During the 3–14-day period after the PRP injection, you may gradually increase physical activity. Please continue to avoid use of NSAIDs; however, ice may be applied for short periods of time throughout the day to aid in management of post-procedure soreness/discomfort if present.
During the 2–4-week period after the PRP, Dr. Best may recommend initiation of a course of physical therapy to aid in recovery and optimization of healing. The patient may begin to note improvement in pain during this time period, though it often takes 1 month or more for the benefits of PRP to take hold.
At this time, PRP injections are not typically covered by any insurance companies. Pricing and payment options can be discussed with Dr. Best and his team prior to your procedure.
As an alternative to PRP injections, intra-articular hip joint injections with corticosteroid can be performed to help alleviate hip region pain. Using x-ray (fluoroscopic) or ultrasound, a needle is carefully and precisely guided to the hip joint. Once the hip joint capsule has been accessed, a steroid solution is instilled through the needle and into the joint. This helps to decrease inflammation and, subsequently, decreases pain and improves function.
At a Glance
Dr. Craig Best
- Harvard Fellowship-Trained Interventional Spine & Sports Medicine Specialist
- Double Board-Certified in Physical Medicnie & Rehabilitation and Pain Medicine
- Assistant Professor of Physical Medicine & Rehabilitation and Orthopedic Surgery
- Learn more

