Hip Arthritis
What is hip arthritis?
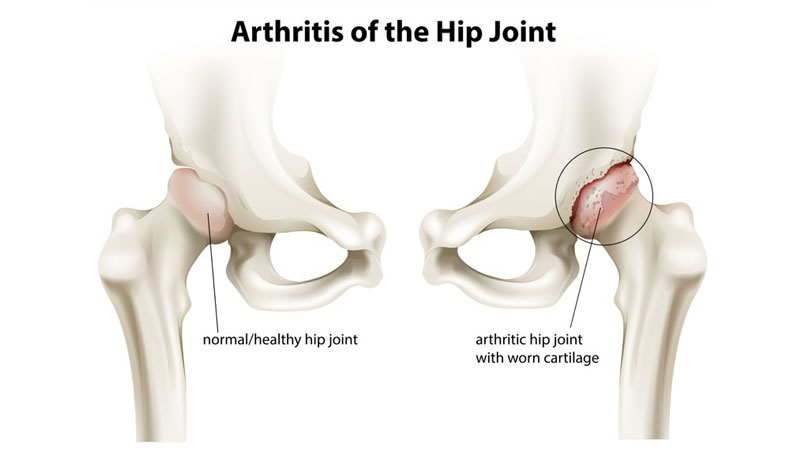
Hip osteoarthritis (OA) results when cartilage that cushions the joint degenerates and deteriorates. This leads to joint inflammation, pain, stiffness, and range of motion limitations. At its end stage, after significant cartilage wear and tear, hip OA may end in bone-on-bone arthritis.
What are risk factors and/or causes of hip arthritis?
Risk of development of hip OA increases with age, obesity, previous joint injuries (e.g. sports injuries, trauma, etc.), and repetitive joint stress imposed by sporting or occupational demands.
How is hip arthritis diagnosed?
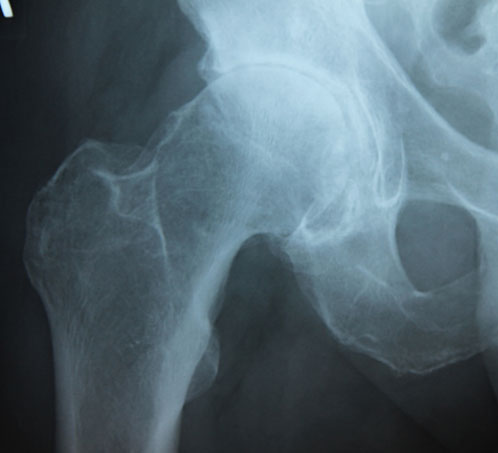
Patients with hip OA typically present with anterior (front) hip and groin pain that is worsened with sitting, standing, or walking. Pain may also be experienced at the posterior (back or buttock) or lateral (side or trochanteric) hip regions. Physical examination may demonstrate limited and painful hip range of motion and positive hip impingement signs. X-ray, computed tomography (CT), or magnetic resonance imaging (MRI) may aid in confirmation of diagnosis. Finally, a diagnostic injection of local anesthetic into the hip joint may help delineate between intra-articular and extra-articular hip pathology.
How is hip arthritis treated?
Initial treatment options for management of hip arthritis may include medications and physical therapy. Physical therapy should primarily focus on multi-planar hip, gluteal, and core strength and stability. If a patient is still experiencing significant pain despite the aforementioned treatment options, interventional options may include corticosteroid or platelet rich plasma (PRP) injections. Finally, referral to orthopedic surgeon skilled in hip replacement (arthroplasty) may be considered for further evaluation and consideration of surgical intervention.
Hip Joint Injection
Using x-ray (fluoroscopic) or ultrasound, a needle is carefully and precisely guided to the hip joint. Once the hip joint capsule has been accessed, a steroid solution is instilled through the needle and into the joint capsule to coat or bathe the joint with anti-inflammatory medication. This helps to decrease inflammation and, subsequently, decreases pain and improves function.
Hip Joint Hyaluronic Acid Injection
Using x-ray (fluoroscopy) or ultrasound, a needle is carefully and precisely guided to the hip joint. Once the hip joint capsule has been accessed, hyaluronic acid is instilled through the needle and into the joint. Hyaluronic acid is a component of synovial (joint) fluid and provides viscosity and elasticity. It may also have anti-inflammatory properties. This allows for restoration of joint lubrication and shock absorbing capacity with subsequent reduction in pain and improved overall joint function.
Platelet Rich Plasma (PRP)
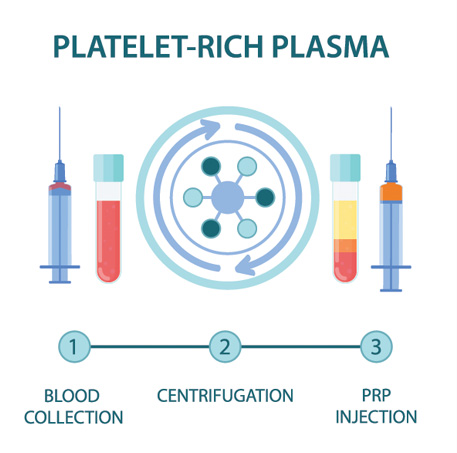
PRP is component of the patient’s own blood. It is rich in growth factors and other cells that signal an increased healing response to a damaged tissue. It is used to treat a variety of painful spine and musculoskeletal conditions.
Blood is drawn from a patient and then placed in a centrifuge for it to be “spun down.” This causes the different components of the blood to separate out in the vial. The PRP solution is then drawn up into a syringe and prepared to be injected at the site of the patient’s injury.
Discontinue use of all non-steroidal anti-inflammatory drugs (NSAIDs) at least 7 days prior to the procedure. These may include ibuprofen (Advil, Motrin), naproxen (Aleve), meloxicam (Mobic), diclofenac (Voltaren), indomethacin (Indocin), and celecoxib (Celebrex). If you are taking oral corticosteroids such as prednisone or a Medrol Dosepak, please discuss this with Dr. Best prior to your procedure. In some cases, Dr. Best may request that the corticosteroid medication be discontinued in preparation for the PRP injection. Do NOT stop aspirin unless specifically instructed by Dr. Best. Depending which body part is injected, you may need a driver to and from your procedure. If you have any questions or concerns about whether to continue or discontinue any of your medications leading up to your PRP injection, please discuss these issues with Dr. Best and his team.
Once the PRP solution is created, the patient is positioned for the procedure. The skin is thoroughly cleaned and the target for the injection obtained with ultrasound or fluoroscopy (x-ray). Then, a numbing solution is injected at the skin and subcutaneous tissues for increased procedural comfort. Finally, under ultrasound or fluoroscopic (x-ray) guidance, the needle is guided to the injury site and the PRP solution is deposited.
It is common to experience mild to moderate pain or discomfort during the initial 0-3 days after the PRP procedure. Post-procedure pain can be easily managed with acetaminophen (Tylenol) or other non-NSAID pain medication. Try to avoid applying ice or heat to the injection site.
During the 3–14-day period after the PRP injection, you may gradually increase physical activity. Please continue to avoid use of NSAIDs; however, ice may be applied for short periods of time throughout the day to aid in management of post-procedure soreness/discomfort if present.
During the 2–4-week period after the PRP, Dr. Best may recommend initiation of a course of physical therapy to aid in recovery and optimization of healing. The patient may begin to note improvement in pain during this time period, though it often takes 1 month or more for the benefits of PRP to take hold.
At this time, PRP injections are not typically covered by any insurance companies. Pricing and payment options can be discussed with Dr. Best and his team prior to your procedure.
As an alternative to PRP injections, intra-articular hip joint injections with corticosteroid can be performed to help alleviate hip region pain. Using x-ray (fluoroscopic) or ultrasound, a needle is carefully and precisely guided to the hip joint. Once the hip joint capsule has been accessed, a steroid solution is instilled through the needle and into the joint. This helps to decrease inflammation and, subsequently, decreases pain and improves function.
At a Glance
Dr. Craig Best
- Harvard Fellowship-Trained Interventional Spine & Sports Medicine Specialist
- Double Board-Certified in Physical Medicnie & Rehabilitation and Pain Medicine
- Assistant Professor of Physical Medicine & Rehabilitation and Orthopedic Surgery
- Learn more

