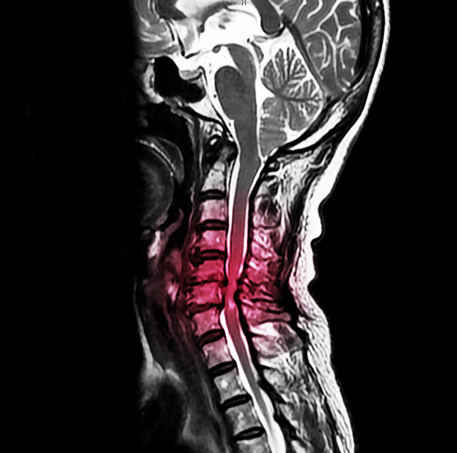
Cervical Spinal Stenosis
What is cervical spinal stenosis?
In general, cervical spinal stenosis represents a variety of structural changes that denote narrowing of the space within the bony spinal column where the spinal cord and/or nerve roots are located. There can be narrowing (stenosis) in the central spinal canal where the spinal cord is located, which is called central canal stenosis. Alternatively, there can be narrowing of the spaces on the sides of the spinal canal (foramen or foramina) where the nerve roots that branch off of the spinal cord exit before then moving toward the upper limb. Central and/or foraminal stenosis and resulting spinal cord and/or nerve root impingement can cause a variety of symptoms such as pain, weakness, numbness, or tingling at the neck and into the upper limb. At its more advanced stages, central canal stenosis can cause such severe spinal cord compression that people may then develop, in addition to the aforementioned symptoms, balance impairment, hand dexterity impairment, and even bladder/bowel incontinence. The constellation of clinical findings is called a cervical myelopathy.
What causes cervical spinal stenosis?
In most cases, the development of cervical spinal stenosis is multifactorial. With time, disc bulges or herniations, malalignment of the vertebral segments (spondylolisthesis), osteophyte (bone spur) formation, joint enlargement (hypertrophy), and ligamentum flavum thickening may all gradually contribute to narrowing the spinal canal. In addition, some people are born with shorter pedicles and, thus, are considered to have congenital spinal stenosis. Finally, in rare instances in which a person suffers a significant acute injury, a large disc herniation may cause a more rapid onset cervical spinal stenosis.
How is cervical spinal stenosis diagnosed?
A diagnosis of cervical spinal stenosis is primarily based on a patient’s symptoms and physical examination findings. Typical symptoms and signs of cervical stenosis include neck pain with radiation of pain to the upper trapezius, shoulder blade (scapula), shoulder, or upper limb. Additionally, there may be associated weakness, numbness, tingling, or reflex changes. Finally, advanced imaging (MRI or CT) and/or electrodiagnostic testing (EMG/NCS) may help to further solidify the diagnosis.
How is cervical spinal stenosis treated?
Initial treatment options for management of pain due to cervical foraminal stenosis causing cervical radiculopathy/radiculitis may include medications, physical therapy, and/or chiropractic. In many cases, these conservative measures will allow for good recovery. If a patient is still experiencing significant pain despite the aforementioned treatment options, a cervical epidural steroid injection (ESI) can be considered as the next step in the treatment pathway. Finally, when all typical non-operative treatments have been exhausted and a patient is still experiencing significant pain, a referral to spine surgery may be considered for further evaluation and possible surgical intervention.
In cases where there is severe central stenosis, referral to spine surgery is typically considered much earlier in the treatment pathway.
Epidural Steroid Injection
When patients with cervical radiculopathy/radiculitis due to disc herniation have not significantly improved with conservative treatments such as medications, physical therapy, or chiropractic care or are unable to tolerate their rehabilitation due to severe pain, an epidural steroid injection (ESI) can be considered. Using x-ray (fluoroscopic), a needle is carefully and precisely guided to the epidural space. Once the epidural space has been accessed, a steroid solution is instilled through the needle and coats the inflamed and painful disc herniation and nerve(s). This helps to decrease inflammation and, subsequently, decreases pain and improves function.

Recent systematic reviews have demonstrated high quality evidence for use of ESIs for management of cervical radicular pain. In the hands of a fellowship-trained interventional spine physician like Dr. Best, ESIs have been found to provide good to excellent improvement in pain in both short- and long-term periods.
While it is not intuitive, studies do not demonstrate any added benefit with a higher dose of steroid. Use of lower dose steroid with an ESI has been shown to be just as effective as moderate and high dose steroid.
As it stands right now, there is no conclusive evidence regarding the number of ESIs that can be performed in a year or a lifetime. However, appropriate spacing between injections and close monitoring of cumulative steroid dosing is important. While a total dose of corticosteroid that a patient receives must be accounted for including oral medications and other injections (e.g. knee injections, shoulder injections), Dr. Best generally limits injections that utilize steroid to 3-4 per 12-month period and separates them out by at least 2-3 weeks.
The response to ESIs can be variable. Some patients may only require one or two ESIs during their entire lifetime to help manage an acute pain issue and may never experience another bout of neck or back pain. Some may experience occasional exacerbations of their cervical or lumbar radicular pain which may require additional injections. The care is tailored to each individual patient and set of circumstances.
The beneficial effects of an ESI usually take effect in 2-7 days after the injection; however, this may be as variable as 1-14 days for some patients.
The large majority of patients do not experience significant side effects from ESIs; however, short-term and generally short-lived side effects may include increase blood sugar (glucose) levels, flushing, insomnia (difficulty sleeping), and gastritis. Long-term side effects of excessive use of steroid may include hypothalamic-pituitary-axis suppression and Cushing’s disease. Dr. Best is mindful of potential excessive corticosteroid administration and is judicious when it comes to this issue.
Steroids administered with ESIs have the potential to increase blood sugar (glucose) levels. On average, blood glucose levels may be increased for one day in non-diabetics and 2 days for diabetics; however, blood glucose levels may be increased for 7-14 days in diabetics. As such, patients with diabetes must do their best to obtain good glucose control prior to an ESI (ideally maintain a hemoglobin A1C less than 7%), monitor their blood glucose levels very closely after undergoing an ESI, and the blood glucose level must be 200mg/dL or less when checking blood glucose level prior to the injection. If an increase in blood glucose levels is noted after undergoing an ESI, it is recommended that the patient contact their primary care physician or endocrinologist to discuss short-term management strategies of the elevated blood glucose levels.
Currently, there is no significant evidence that avoidance of bathing or swimming decreases risk of infection after spine injections; however, we generally ask that patients avoid submerging in water for 24 hours after the injection just to be on the safe side. There are no concerns regarding showers at any point after an ESI.
At a Glance
Dr. Craig Best
- Harvard Fellowship-Trained Interventional Spine & Sports Medicine Specialist
- Double Board-Certified in Physical Medicnie & Rehabilitation and Pain Medicine
- Assistant Professor of Physical Medicine & Rehabilitation and Orthopedic Surgery
- Learn more

