Lumbar Disc Herniation
What is a lumbar disc herniation?
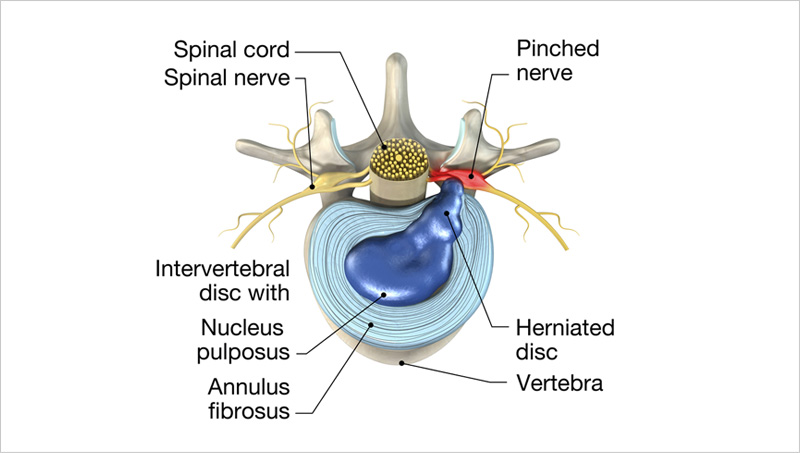
A herniated intervertebral disc refers to a condition in which the more liquid or “jelly-like” inner portion of the disc (nucleus pulposus) pushes through a tear (fissure) in the outer portion of the disc (annulus fibrosus). This can cause an inflammatory reaction at the area of the disc herniation and nearby nerves. In addition, the herniated disc can also cause compression of the nerves. Both of these mechanisms can potentially elicit pain. Additionally, the injury to the disc itself may be a cause of pain.
What causes a lumbar disc herniation?
Most commonly, a disc herniation occurs due to gradual “wear and tear” or degeneration of the disc with weakening and fissuring of the firm, rubbery outer layer of the disc (annulus fibrosus). This allows the “jelly-like” inner portion of the disc (nucleus pulposus) to protrude through the tear (fissure) in the disc and potentially compress a nearby nerve root. In other cases, there may a known accident or trauma such as a motor vehicle collision, work injury, or sports injury. In many cases, however, the patient cannot recall a specific incident or event that led to the onset of their pain.
How is a lumbar disc herniation diagnosed?
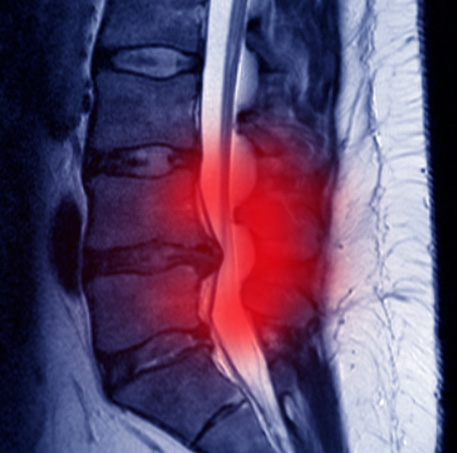
A diagnosis of lumbar disc herniation is primarily based on a patient’s symptoms and physical examination findings. Typical symptoms and signs of lumbar disc herniation include low back pain with or without radiation of pain to the hip, buttock, thigh, or lower limb. Additionally, there may be associated weakness, numbness, tingling, or reflex changes of the lower limb. Finally, advanced imaging (MRI or CT) may help to further confirm and solidify the diagnosis.
How is a lumbar disc herniation treated?
Initial treatment options for management of pain due to a disc herniation may include medications, physical therapy, and/or chiropractic. In many cases, these conservative measures will allow for good recovery. If a patient is still experiencing significant pain despite the aforementioned treatment options, a lumbar epidural steroid injection can be considered as the next step in the treatment pathway. Finally, when all typical non-operative treatments have been exhausted and a patient is still experiencing significant pain, a referral to spine surgery may be considered for further evaluation and possible surgical intervention.
Epidural Steroid Injection
When patients with lumbar radiculopathy/radiculitis due to disc herniation have not significantly improved with conservative treatments such as medications, physical therapy, or chiropractic care or are unable to tolerate their rehabilitation due to severe pain, an epidural steroid injection (ESI) can be considered. Using x-ray (fluoroscopic), a needle is carefully and precisely guided to the epidural space. Once the epidural space has been accessed, a steroid solution is instilled through the needle and coats the inflamed and painful disc herniation and nerve(s). This helps to decrease inflammation and, subsequently, decreases pain and improves function.

Recent systematic reviews have demonstrated high quality evidence for use of ESIs for management of lumbar radicular pain. In the hands of a fellowship-trained interventional spine physician like Dr. Best, ESIs have been found to provide good to excellent improvement in pain in both short- and long-term periods.
While it is not intuitive, studies do not demonstrate any added benefit with a higher dose of steroid. Use of lower dose steroid with an ESI has been shown to be just as effective as moderate and high dose steroid.
As it stands right now, there is no conclusive evidence regarding the number of ESIs that can be performed in a year or a lifetime. However, appropriate spacing between injections and close monitoring of cumulative steroid dosing is important. While a total dose of corticosteroid that a patient receives must be accounted for including oral medications and other injections (e.g. knee injections, shoulder injections), Dr. Best generally limits injections that utilize steroid to 3-4 per 12-month period and separates them out by at least 2-3 weeks.
The response to ESIs can be variable. Some patients may only require one or two ESIs during their entire lifetime to help manage an acute pain issue and may never experience another bout of neck or back pain. Some may experience occasional exacerbations of their cervical or lumbar radicular pain which may require additional injections. The care is tailored to each individual patient and set of circumstances.
The beneficial effects of an ESI usually take effect in 2-7 days after the injection; however, this may be as variable as 1-14 days for some patients.
The large majority of patients do not experience significant side effects from ESIs; however, short-term and generally short-lived side effects may include increase blood sugar (glucose) levels, flushing, insomnia (difficulty sleeping), and gastritis. Long-term side effects of excessive use of steroid may include hypothalamic-pituitary-axis suppression and Cushing’s disease. Dr. Best is mindful of potential excessive corticosteroid administration and is judicious when it comes to this issue.
Steroids administered with ESIs have the potential to increase blood sugar (glucose) levels. On average, blood glucose levels may be increased for one day in non-diabetics and 2 days for diabetics; however, blood glucose levels may be increased for 7-14 days in diabetics. As such, patients with diabetes must do their best to obtain good glucose control prior to an ESI (ideally maintain a hemoglobin A1C less than 7%), monitor their blood glucose levels very closely after undergoing an ESI, and the blood glucose level must be 200mg/dL or less when checking blood glucose level prior to the injection. If an increase in blood glucose levels is noted after undergoing an ESI, it is recommended that the patient contact their primary care physician or endocrinologist to discuss short-term management strategies of the elevated blood glucose levels.
Currently, there is no significant evidence that avoidance of bathing or swimming decreases risk of infection after spine injections; however, we generally ask that patients avoid submerging in water for 24 hours after the injection just to be on the safe side. There are no concerns regarding showers at any point after an ESI.
At a Glance
Dr. Craig Best
- Harvard Fellowship-Trained Interventional Spine & Sports Medicine Specialist
- Double Board-Certified in Physical Medicnie & Rehabilitation and Pain Medicine
- Assistant Professor of Physical Medicine & Rehabilitation and Orthopedic Surgery
- Learn more

